Validation of the Mortality in Emergency Department Sepsis (MEDS) Score in Patients with SIRS
Validation of the Mortality in Emergency Department Sepsis (MEDS) Score in Patients with the Systemic Inflammatory Response Syndrome (SIRS).
INTRODUCTION:
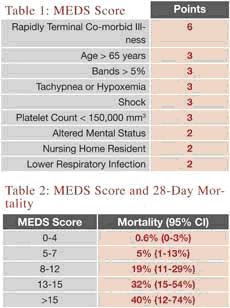
Because 40% of ICU patients with sepsis are admitted from the ED, a prognostic screening instrument derived and validated on this unique population could focus resource allocation towards those most likely to benefit. Although multiple instruments have been developed for ICU patients, few have been validated in the ED setting. In the current study, admitted ED patients with SIRS criteria at one of four geographically disparate university hospitals were prospectively recruited. Research assistants, not clinicians, collected the MEDS variables which were not disclosed to or utilized by the treating physician. Among the 385 enrolled patients, 9% died and 11% required mechanical ventilation. The primary outcome was 28-day mortality as ascertained by telephone follow-up or hospital record review.The MEDS score was derived in 2003 and is a nine-component instrument (Table 1) which has been validated in multiple settings demonstrating increasing mortality as the score increases (Table 2). Additionally, each MEDS variable has demonstrated at least moderate reliability meaning that if two physicians use the MEDS to risk-stratify the same patient they will likely obtain the same score. Finally, when compared head-to-head, MEDS compares favorably to other scoring systems and to serum lactate levels.
The Caveats:
While the MEDS score is a Level II Clinical Decision Rule validated for wide-spread use across varied ED settings, no impact analysis has been performed. In other words, in actual clinical practice nobody knows if physicians or patients will accept this rule, appropriately apply and interpret it, or if MEDS will alter patient-important outcomes such as inappropriate, risky therapy or mortality. In fact, recent research has suggested that MEDS may not reliably risk-stratify the sickest septic patients. However, the more severely ill septic patients, defined as fluid-refractory hypotension. Others have retrospectively identified APACHE II, SAPS and MPM as superior tools. None of these instruments were prospectively derived or validated upon ED patients, though. Future research should combine the MEDS score with clinical gestalt, in addition to an ever-expanding array of sepsis biomarkers (lactate, C-reactive protein) to further assess and perhaps enhance this prognostic tool.
Your patient has persistent hypotension despite your early goal directed therapy saline bolus of 20 mL/kg and you subsequently note hypoxia accompanying a pulmonary infiltrate. Unfortunately, your hospital performs automated CBC so bandemia is never reported, though you suspect he might manifest bands given his WBC 27,000. Nonetheless, his age, persistent hypotension, hypoxia, and confusion still net him a MEDS score of 11. Your critical care colleagues are called immediately after his chest x-ray and blood counts return. Provided his diagnosis and MEDS score, they admit him without argument and he is en route to the ICU within 90-minutes of ED arrival.


Comments